+ Anatomy
- Thyroid glands consist of 2 distinct lobes located lateral and ventral to the 5th-8th tracheal rings
- Thyroid gland in cats: 10-20 mm long, 3-4 mm wide, and 2 mm thick
- Isthmus may connect right and left thyroid glands
- Parathyroid glands are salmon-coloured and distinct from the thyroid glands
- 1 external and 1 internal parathyroid gland per thyroid gland
- External parathyroid gland is on the cranial pole of the thyroid gland and external to its capsule
- Internal parathyroid gland are within the thyroid capsule in the caudal and medial aspects of the thyroid
- Cranial thyroid artery is a branch of the common carotid artery and provides the majority of arterial supply to dogs
- Caudal thyroid artery is a branch of the brachiocephalic artery and unites with the cranial thyroid artery in the loose areolar tissue along the dorsomedial surface of the thyroid capsule and provides some arterial supply to dogs
- External parathyroid gland is vascularized by a branch of the cranial thyroid artery
- Venous drainage is through the cranial and caudal thyroid veins
- Innervation: thyroid nerve from the recurrent laryngeal nerve dorsomedial to thyroid glands
- Ectopic thyroid tissue is common and can be located anywhere from the base of the tongue to the heart base
FELINE HYPERTHYROIDISM
+ Pathophysiology
es include regional lymph nodes (i.e., submandibular and retropharyngeal) and lungs, but other sites include adrenal glands, brain, kidneys, heart, liver, and bone
- Thyroid carcinoma can also arise from ectopic tissue in tongue, ventral neck, and cranial mediastinum
+ Clinical Signs
- Clinical signs due to stimulatory effects of excessive thyroid hormones on various organ systems
- Clinical severity depends on duration of hyperthyroidism, presence of concurrent diseases, and ability to meet increased demands imposed by excessive thyroid hormone secretion
- Laryngeal hemiparesis in a cat has been reported to result from peripheral compression of the recurrent laryngeal nerve by a functional cystic thyroid adenoma
- Polyuria and polydipsia is common (36%-60%) due to increased renal perfusion reducing renal medullary solute concentration or secondary to direct thyrotoxic effect on hypothalamus
- Panting due to decreased pulmonary compliance and increased minute respiration resulting from respiratory muscle weakness and increased CO 2 production
- Other clinical signs include weight loss, polyphagia, vomiting, increased activity, restlessness, diarrhea, and weakness
DIAGNOSIS
+ Physical Examination
- Palpable enlargement in 1 or both thyroid glands is most significant clinical finding
- Failure to palpate thyroid glands may result from ventral descent of the thyroid glands into the thoracic inlet or adenomatous or malignant changes in ectopic tissue
- Thyroid glands may be palpable without clinical or laboratory evidence of hyperthyroidism, but these adenomatous changes will become functional
- Other physical examination findings include thin body condition, tachycardia, heart murmur, gallop rhythm, and unkempt hair coat
+ Laboratory Findings
- Increased serum levels of thyroid hormone concentrations with resting T 4 levels above normal ranges
- 25% of **hyperthyroid cats have normal T 3 levels with elevated T 4 levels and clinical signs are usually mild
Normal serum thyroxine concentrations can occur in hyperthyroid cats as:
- T 4 levels can fluctuate in and out of reference range with mild hyperthyroidism
- Concurrent non-thyroid illness may suppress serum thyroxine levels to the high normal range
- Provocative tests, using exogenous thyrotropin-releasing hormone or TSH, are being investigated as a means of diagnosing hyperthyroidism with borderline T 4 blood levels
- T 3 suppression test may be a more reliable method for confirming hyperthyroidism
- Exogenous T 3 will normally result in a negative feedback on the hypothalamus-pituitary-thyroid axis causing inhibition of TSH release and decreased endogenous thyroid hormone secretion
- thyroid secretion is autonomous and independent of TSH regulation in hyperthyroid cats and hence exogenous T 3 will not effect serum thyroid hormone concentrations
- Hematology: mature leukocytosis and neutrophilia, eosinopenia, and a mild to moderate erythrocytosis
- Serum biochemistry: elevated ALP, ALT, BUN, and creatinine
- mild to moderate renal compromise can be masked by increased GFR secondary to hyperthyroidism
- Renal blood flow, GFR, and tubular reabsorption are decreased in cats with hyperthyroidism
+ Cardiac Evaluation
- cardiac abnormalities (i.e., tachycardia > 220 beats per minute, gallop rhythm, or sternal murmur) should be assessed with ECG, thoracic radiographs, and echocardiogram
Radionucleide Imaging
- Nuclear scintigraphy provides an image of function thyroid tissue
- Nuclear scintigraphy of the thyroid gland commonly involves technetium Tc 99m pertechnetate and 2 isotopes of radioactive iodine (i.e., 131I and 123I)
- Radioactive iodine is preferentially concentrated in the thyroid gland where it is bound and incorporated into tyrosine residues of thyroglobulin
- Pertechnetate is trapped by the thyroid gland, but not bound to thyroglobulin or stored in the thyroid gland
- Pertechnetate is preferred for diagnostic imaging because of low cost, short half-life, low radiation dose, and equal to superior image quality compared to the iodine radionucleides
- Furthermore, hyperthyroid medication does not interfere with pertechnetate imaging and does not need to be discontinued prior to imaging
Medical Management
+ General Considerations
- Aim: control excessive thyroid hormone secretion from hyper-functioning thyroid gland
Management options:
- Oral ± transdermal antithyroid medical therapy
- Radioactive iodine administration
- ± intralesional ultrasound-guided ethanol injection or radiofrequency heat ablation
- Surgical thyroidectomy
Therapeutic options depend on age, concurrent cardiovascular and renal disease, availability of nuclear medicine facilities, skill of the surgeon, and owner compliance
Drugs that interfere with thyroxine synthesis are effective as hyperthyroidism is caused by hyper-functional thyroid tissue
- Carbimazole is converted to methimazole
- Methimazole interferes with iodination of thyroglobulin (i.e., thyroxine precursor in thyroid follicles)
- Dose for both carbimazole and methimazole: 10-15 mg/day PO
- Carbimazole and methimazole do not decrease size of thyroid glands, but T 4 levels decrease to normal < 3 weeks
- Lowest dose possible should be used for long-term management by decreasing methimazole dose in 2.5 mg increments and repeating T 4 testing every 2-3 weeks to determine the lowest possible dose which maintains T 4 within the normal reference range
- Propylthiourscil is also available, but associated with more severe side-effects
- Complications include:
- Anorexia, nausea, vomiting, and lethargy during the initial periods is common, but transient
- Long-term complications are uncommon and include thrombocytopenia and agranulocytosis
- Tachycardia and cardiac abnormalities can be controlled with carbimazole or methimazole (although minimum 2 weeks for effect) or β-adrenergic antagonists such as propanolol or atenolol
- Propanolol has additional beneficial effects of reducing catecholamine-associated side effects such as anxiety and hypertension
- Propanolol dose: 0.5 mg/kg q 8-12 hrs for 2-5 days
- Atenolol dose: 6.25-12.50 mg/cat/day
+ Radioactive Iodine Treatment
- Simple, effective, and safe method for the treatment of functional feline hyperthyroidism
- Aim: restore euthyroidism and prevent hypothyroidism with a single dose of radiation
- Eadioisotope 131I concentrates primarily in hyperplastic and neoplastic thyroid cells
- Irradiation results in destruction of all hyperplastic and neoplastic tissue including ectopic and metastatic tissue
- 75% of cases are euthyroid < 8 days of a single intravenous treatment
- Radioactive iodine can be administered by intravenous, subcutaneous, or oral routes
- Response to radioactive iodine is reduced by high serum thyroxine concentrations, large thyroid glands, and anti-thyroid drug administration
- Disadvantages: limited availability of nuclear medicine facilities, radiation safety regulations, expense, prolonged hospitalization, and difficulty in determining correct dose
- 2.5% recurrence rate
- MST 2 years, with 1-year survival rate 89%, 2-year survival rate 72%, and 3-year survival rate 52%
+ Percutaneous Ultrasound-Guided Ethanol Injection
- Percutaneous ultrasound-guided treatments include 96% ethanol and radiofrequency heat ablation
- Percutaneous injection of ethanol results in coagulative necrosis and vascular thrombosis
- Percutaneous ethanol injection resulted in normalization of T 4 levels within 24-48 hours and no clinical or diagnostic evidence of recurrence of hyperthyroidism in 12 months in 4 cats with unilateral thyroid masses
- However, percutaneous ethanol injection is not recommended for cats with bilateral thyroid gland enlargement as resolution of clinical signs was transient (up to 27 weeks) and the complication rate was high, including death from non-staged bilateral ethanol injection and Horner's syndrome, dysphonia, laryngeal paralysis, and death
+ Percutaneous Ultrasound-Guided Radiofrequency Heat Ablation
- Radiofrequency treatment causes heat development by agitating local ions and creating friction
- Amount of tissue exposed to heat and the amount of heat created are directly related to tissue impedance
- Relatively small size of the feline thyroid gland and variations in impedance may result in non-uniform and incomplete tumor destruction
- Percutaneous ultrasound-guided radiofrequency heat ablation in cats with bilateral thyroid enlargement results in a transient decrease of T 4 levels within 24-48 hours
- However, hyperthyroidism recurred in all cats with a mean DFI of 4 months (range, 0-18 months)
- Adverse effects: transient Horner's syndrome and laryngeal paralysis
Surgical Management
+ General Considerations
- Surgery is effective and relatively simple, but can be associated with significant morbidity and mortality
- Thyroidectomy is curative and normalizes serum thyroxine concentrations within 48 hours
- Thyroidectomy techniques include:
- Intracapsular and modified intracapsular thyroidectomy
- Extracapsular and modified extracapsular thyroidectomy
- Staged bilateral thyroidectomy procedures
- Aim: remove abnormal thyroid tissue and preserve at least 1 parathyroid gland
- Bilateral adenomatous hyperplastic tissue is identified in 70% of functional hyperthyroid cats
- Extent of thyroid involvement should be predetermined with nuclear scintigraphy if possible as 15% of hyperplastic tissue appears grossly normal
- Disadvantages: anesthetic risk, difficult intraoperative assessment of abnormal tissue, 9% mortality rate, and post-surgical complications such as hypoparathyroidism, recurrence, and hypothyroidism
- Recurrence of hyperthyroidism following unilateral thyroidectomy within 12 months
+ General Anesthesia
- Cats should be treated with methimazole preoperatively for 2-3 weeks to achieve an euthyroid state
- Propanolol (0.4-1.2 mg/kg q 12 hr) or atenolol (6.25 mg/kg q 24 hr) can be used preoperatively for 1-2 weeks if methimazole is not tolerated to decrease heart rate and control hypertension and myocardial hyperexcitability
- β-blockers are not used in cats with CHF until heart failure is stabilized using diuretics and other medication
- Premedication and general anesthetic agents with minimal cardiac arrhythmic effects are preferred
- Premedication with acepromazine reduces the autonomic manifestations of hyperthyroidism and prevents arrhythmias induced by thiobarbiturates and inhalation agents
- Xylazine potentates cardiac arrhythmias
- Anticholinergic agents stimulate adrenergic activity and result in tachycardia and arrhythmias
- Ketamine increases sympathoadrenal activity and may cause catecholamine-induced arrhythmias, but some authors recommend ketamine as an induction agent
- Intravenous thiobarbiturates or isoflurane are preferred as they have antithyroid activity
- Thiobarbiturates are arrhythmic and should be administered carefully in emaciated cats
- Isoflurane is recommended for maintenance of anesthesia as halothane and methoxyflurane sensitize the heart to catecholamine-induced arrhythmias
- Intraoperative ECG and anesthetic monitoring is recommended as ventricular arrhythmias are common
+ Surgical Approach
- Position: dorsal recumbency with neck extended and towel placed under neck
- Ventral midline skin incision from larynx to the manubrium
- Skin incision continued through subcutaneous tissue and oblique fibres of sphincter coli muscle
- Sternohyoideus muscles are exposed and separated in midline to expose trachea
- Thyroid glands normally located immediately caudal to larynx on medial aspect of sternothyroideus muscles
- However, abnormal thyroid glands can be located ventral or lateral to trachea anywhere between larynx and thoracic inlet
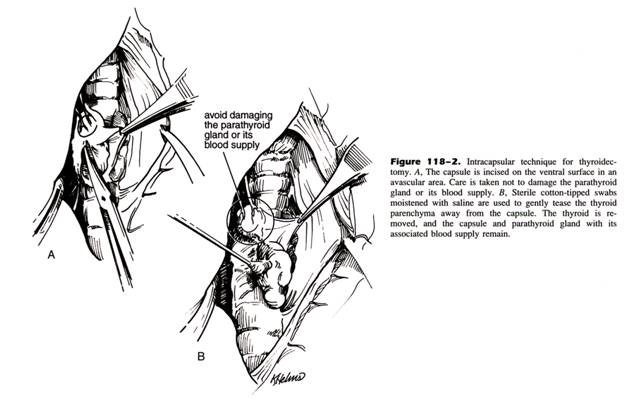
+ Intracapsular Thyroidectomy
- Intracapsular techniques preserve the thyroid capsule and external parathyroid gland
- Longitudinal incision with scalpel blade or fine iris scissors through ventral aspect of thyroid capsule
- Saline-soaked cotton bud used to tease thyroid gland away from inside aspect of thyroid capsule
- External parathyroid gland and delicate blood supply are preserved
- Advantages: technically simple with preservation of a parathyroid gland decreasing the risk of hypocalcemia
- Complications: recurrent hyperthyroidism (8%-22%) due to retained remnants of abnormal thyroid tissue
- Incidence of hypoparathyroidism reduced compared with extracapsular techniques with 15%-26% transient hypocalcemia due to disruption of parathyroid blood supply
From: Slatter DH (ed): Textbook of Small Animal Surgery (3rd ed).
+ Modified Intracapsular Thyroidectomy
- Modification of intracapsular technique with thyroid capsule resected following removal of thyroid gland leaving small rim of thyroid capsule around external parathyroid gland
- Recurrence rate: 0%-5%
- Complication: increased risk of hypocalcemia (33%-36%)
+ Extracapsular Thyroidectomy
- Extracapsular techniques remove the thyroid gland and its capsule, but is not recommended for cats with bilateral disease because of a high incidence of hypoparathyroidism
- Cranial thyroid artery and cranial and caudal thyroid veins ligated and divided
- Complications: hypoparathyroidism (11%-82%) and recurrence (0%-9%)
- Parathyroid gland should be minced and re-implanted into adjacent muscle for revascularization and possible return to normal function if compromised as autotransplantation of parathyroid tissue results in a more rapid return to normocalcemia and decreased overall morbidity
+ Modified Extracapsular Thyroidectomy
- Modification of extracapsular thyroidectomy
- Thyroid capsule incised approximately 300º around external parathyroid gland
- External parathyroid gland and surrounding thyroid capsule are gently dissected away from the remainder of the thyroid capsule and gland
- Caudal thyroid vein is ligated and divided
- Thyroid gland and approximately 90% of thyroid capsule is removed leaving small rim of thyroid capsule around external parathyroid gland
- Complications: hypocalcemia (23%) and recurrence (4%)

From: Slatter DH (ed): Textbook of Small Animal Surgery (3rd ed).
+ Bilateral Thyroidectomy
- Bilateral thyroidectomy recommended regardless of gross size or appearance by some investigators
- Bilateral thyroidectomy techniques include single stage or staged procedures ± parathyroid implantation
Complications include:
- Hypothyroidism, but thyroid levels may return normal
- Recurrence (0%) and hypocalcemia (0%-4%) are rare
Postoperative Management
+ Hypocalcemia
- Hypocalcemia is the most significant complication of thyroidectomy
- 77% cats with hyperthyroidism are also hyperparathyroid and reversal of hyperthyroidism may predispose cats to hypoparathyroidism and hypocalcemia in postoperative period
- Serum calcium levels should be monitored especially after bilateral thyroidectomy
- Hypocalcemia occurs most commonly 2-5 days following surgery
- Clinical signs occur when serum calcium concentration < 7.5 mg/dL
- Clinical signs: restlessness, weakness, muscle tremors, twitching, tetany, and seizures
- Treatment of hypocalcemia includes:
- 10% calcium gluconate (0.5-1.5 mg/kg IV) at over 10-20 minutes initially
- 10% calcium gluconate (10 ml added to 250 ml maintenance solution) at 60 ml/kg/day
- Maintenance with oral calcium gluconate (3-4 ml diluted 1:1 with isotonic saline q 6-8 hrs or 0.2-0.5 g/cat)
- Maintenance with vitamin D (0.02-0.03 mg/kg q 24 hr PO for 5-7 days)
- Vitamin D supplementation can eventually be tapered and withdrawn in the majority of cats
- Permanent hypoparathyroidism is likely if calcium does not return to normal within 14 days
- Spontaneous resolution of hypoparathyroidism due to reversible damage or hypoxia resulting from thyroidectomy or compensation by accessory parathyroid tissue
+ Hypothyroidism
- Thyroxine supplementation is rarely required after unilateral thyroidectomy despite subnormal T 4 levels
- Serum T 4 concentrations should be reassessed annually
+ Recurrence of Hyperthyroidism
- Recurrence of hyperthyroidism is caused by the inability to remove all abnormal thyroid tissue, failure to recognize abnormal tissue, presence of either abnormal ectopic tissue or metastases and redevelopment of hyperplastic adenomatous tissue in the remaining thyroid gland
- Medical or radioactive iodine therapy is recommended for recurrent hyperthyroidism
+ Other Complications
- Dyspnea and laryngeal paralysis resulting from intraoperative damage to the recurrent laryngeal nerve
- Horner's Syndrome resulting from intraoperative damage to the cervical sympathetic trunk
- Hemorrhage
+ Feline Thyroid Adenocarcinoma
- Thyroid ADC is a rare cause of feline hyperthyroidism (2%-11%)
- No significant difference in T 4 levels between benign and malignant thyroid neoplasia
- Malignant thyroid ADC is characterized by patchy or irregular uptake on nuclear scintigraphy, multiple and fixed thyroid masses, and frequent recurrence of clinical signs
- Metastatic rate up to 71%
- Treatment: surgical resection and radioactive iodine therapy ± external beam radiation therapy
- Prognosis: survival time ranging from 10-41 months in 7 cats


