GENERAL CONSIDERATIONS
+ Location
- Spinal cord tumors are classified as extradural, intradural-extramedullary, or intramedullary
- Extradural tumors are most common and account for 50% of spinal tumors
- Intradural-extramedullary account for 30% and intramedullary account for 15% of spinal tumors
+ Signalment
- 90% of spinal tumors occur in large breed dogs
- 28% of spinal tumors occur in cats and dogs < 3 years
Canine Spinal Cord Tumors
+ General Considerations
- Spinal cord tumors are uncommon in dogs
- Meningioma is the most common with a predilection for the cervical spinal cord
- Other primary tumors include LSA, MCT, and intradural-extramedullary spinal cord tumor of young dogs
- HSA is the most common metastatic tumor, but others include pilomatrixoma and pheochromocytoma
+ Extradural Spinal Cord Tumors
- Primary vertebral tumors and multiple myeloma
- Other extradural tumors include myxoma, myxosarcoma, LSA, and lipoma or liposarcoma
+ Intradural-Extramedullary Spinal Cord Tumors
- Meningioma and peripheral nerve sheath tumors are the most common intradural-extramedullary tumors
- Spinal meningioma accounts for 14% of all CNS meningioma
- Spinal meningioma has a predilection for the cervical spinal cord:
- 40%-77% cervical spinal cord
- 0%-32% thoracic spinal cord
- 23%-28% lumbar spinal cord
- Peripheral nerve sheath tumors involve the spinal cord in 65% cases
- Other intradural-extramedullary tumors include hemangioma (common), myxoma, myxosarcoma, and an unusual case of diffuse meningeal tumor affecting entire meningeal surface of CNS
+ Intradural-Extramedullary Spinal Cord Tumor of Young Dogs
- Uncommon
- Synonyms: ependymoma, neuroepithelioma, spinal cord blastoma, medulloepithelioma, hamartoma, and nephroblastoma
- Age: 6 months to 3 years
- Breed predisposition: GSD, Labrador Retriever, and Golden Retriever
- Clinical signs: lateralized with vast majority of lesions between T10-L2
- Microscopically similar to nephroblastoma and some believe this tumor may represent extrarenal nephroblastoma arising from ectopic mesonephric or metanephric tissue trapped within the dura during embryologic development
- Diagnosis: CSF findings are usually non-specific, but albuminocytologic dissociation may be consistent with a chronic neoplastic process
- Treatment: cytologic reduction or removal associated with long-term survival (4 months and > 3 years) ± radiation therapy for incompletely excised tumors
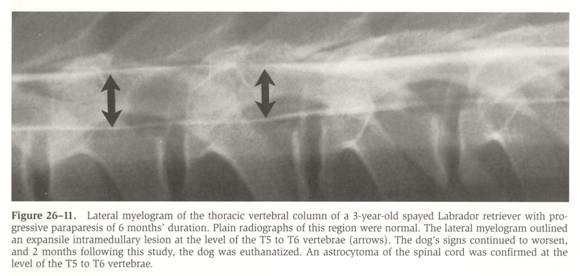
+ Intramedullary Spinal Cord Tumors
- Intramedullary spinal cord tumors are uncommon
- Intramedullary spinal cord tumors usually have glial cell origin: astrocytoma, oligodendroglioma, undifferentiated sarcoma, ependymoma, and choroid plexus papilloma
- Intramedullary spinal cord tumors are most commonly located between C6-T2
- Intramedullary spinal cord metastasis can also occur before evidence of the primary tumor
- Primary tumors with a propensity for metastasizing to the spinal cord include HSA and LSA ± mammary ADC and malignant melanoma
- Malformation tumors may also affect the spinal cord parenchyma such as epidermoid cyst and hamartoma
CLINICAL FEATURES
+ History
- Extradural spinal cord tumors are usually slow growing and progressive over weeks to months
- Acute onset of neurologic signs may be caused by tumor-induced hemorrhage or ischemia
- Intramedullary tumors have a more rapid growth rate and have a higher incidence of hemorrhage, ischemia, and necrosis
+ Clinical Signs
- Clinical signs depend on the tumor location and are difficult to differentiate from other causes of myelopathy
- Extradural tumors may involve the meninges, spinal nerves, or nerve roots which results in varying levels of pain from discomfort to extreme spinal hyperesthesia
- Tumors involving the brachial or lumbar intumescence may cause lameness, limb elevation, neurogenic muscle atrophy, and depressed spinal reflexes
- Hyperesthesia is associated with extradural and intradural-extramedullary tumors, but not intramedullary tumors
- Fundus, lymph node, and rectal examination should be performed for evidence of LSA or metastatic lymphadenopathy
DIAGNOSIS
+ Survey Radiographs
- Thoracic radiographs for evaluation of metastatic disease
- Radiographic findings include cortical lysis with collapse of the adjacent intervertebral disk space
- Vertebral body and dorsal lamina are more frequently affected than dorsal and transverse spinous processes
- Radiographic signs not always visible due to inconsistent vertebral shape, overlying ribs and soft tissue, and improper positioning
- Cortical bone destruction is a late event in metastatic vertebral lesions
- Radiographic abnormalities associated with non-vertebral spinal cord tumors are rare, but slow and progressive tumor growth may cause enlargement of an intervertebral foramen or vertebral canal with thinning of cortical bone
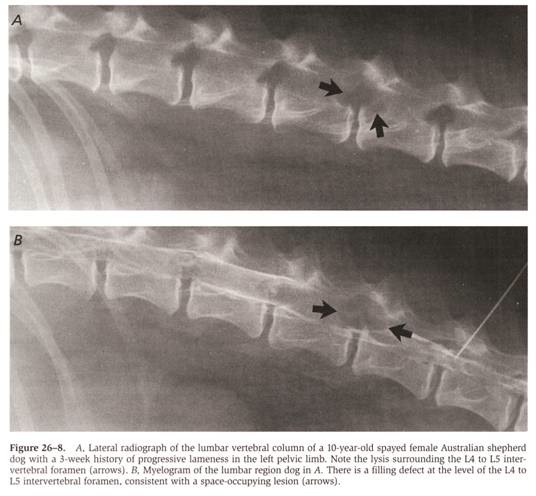 From: Withrow SJ & MacEwen EG (eds): Small Animal Clinical Oncology (3rd ed).
From: Withrow SJ & MacEwen EG (eds): Small Animal Clinical Oncology (3rd ed).
+ Cerebrospinal Fluid Analysis
- CSF collection and analysis are recommended if survey radiographs are inconclusive
- CSF is collected from a lumbar site and needle left in situ for myelography
- CSF changes include increased protein content and normal to increased white cell count
- CSF findings with LSA include increase white cell count with abnormal lymphocytes
- Abnormal CSF findings are more common in dogs with spinal LSA due to leptomeningeal involvement
+ Myelography
- Indications: determining presence, anatomical location and dural site of spinal cord tumor
- Spinal cord tumors are classified as extradural, intradural-extramedullary, or intramedullary
- Classification may be difficult due to spinal cord edema
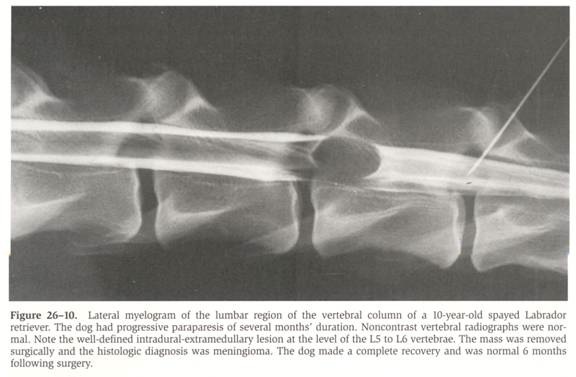
 From: Withrow SJ & MacEwen EG (eds): Small Animal Clinical Oncology (3rd ed).
From: Withrow SJ & MacEwen EG (eds): Small Animal Clinical Oncology (3rd ed).
+ Advanced Imaging
- CT is recommended for vertebral tumors due to excellent bone detail
- However, myelography is superior to CT in differentiating intramedullary from intradural-extramedullary
- MRI is recommended for spinal cord tumors due to excellent soft tissue detail
- MRI provides accurate information on anatomic location and bone involvement, but differentiation between intradural, extradural and intramedullary, and extramedullary difficult
Treatment
+ General Considerations
- Management options depends on tumor location, extent, and histologic type
- Aim: alleviate spinal cord compression
- Treatment options include conservative (with corticosteroids) and surgery
- Surgery allows decompression ± complete removal or cytoreduction of the mass
- Surgical decompression techniques include hemilaminectomy and dorsal laminectomy
- Complete resection of spinal meningioma is complicated by adhesions to the pia mater or spinal cord, and friable texture resulting in piecemeal dissection
- Rhizotomy can be performed to facilitate tumor resection, but avoided in the brachial and lumbar intumescence
- Radiation therapy can be used for LSA, incompletely resected spinal tumors, and when surgery is not feasible
- Spinal cord is resistant to the acute effects of radiation due to low replication rate, but late effects (> 2 years) can be seen due to progressive demyelination and malacia of white matter (especially oligodendrocytes, endothelial cells, astrocytes, and microglial cells)
PROGNOSIS
+ General Considerations
- Prognosis depends on resectability, histologic type, location, and severity of neurologic signs
- Poor prognosis for metastatic and vertebral tumors
+ Surgery
- Guarded to good prognosis for intradural-extramedullary lesions following surgical resection
- Overall MST 240 days for surgically resected spinal cord tumors:
- MST 180 days for malignant spinal tumors
- MST 1,410 days for benign spinal tumors
- 56% dogs with spinal meningioma alive > 6 months
- Poor prognostic factors for spinal meningioma include tumors located in either the cervical or lumbar intumescence, ventral tumors, and iatrogenic cord trauma during dissection
+ Radiation Therapy
- Guarded to good prognosis for intramedullary tumors treated with radiation therapy with normal spinal cord tolerating radiation well and neurologic signs alleviated > 1 year
- MST 17 month MST for intradural-extramedullary and intramedullary tumors following cytoreductive surgery and radiation therapy


