+ General Considerations
- Mammary tumors are the most common tumor in female dogs, accounting for 42% of all tumors and 82% of reproductive tumors
- Mean age 6-10 years and rare < 4 years
- Breed predisposition: Pointers, Irish Setter, Brittany Spaniel, English Springer Spaniel, Labrador Retriever, Great Pyrenees, Samoyed, Airedale Terrier, Miniature and Toy Poodle, Dachshund, and Keeshond
- Mammary tumors in male dogs are usually malignant
- Multiple mammary tumors are common: 672 female entire Beagles followed for life-span with 71% having at least 1 mammary tumor and 61% with > 1 mammary tumor
+ Benign Mammary Tumors
- Benign tumors include adenoma (simple, complex, and basaloid), fibroadenoma, mixed tumor, and duct papilloma
- Mixed tumor is common and contains epithelial and mesenchymal components (i.e., cartilage, bone, or fat)
+ Malignant Mammary Tumors
- 41%-53% of mammary tumors in female dogs are malignant
- Life-time risk of female intact dog developing a malignant mammary tumor is 23%-34%
- However, histologic evidence of malignancy does not imply malignant course of disease as only 4.4% cases of malignant mammary carcinoma are fatal
- Revised WHO classification of malignant mammary tumors ranks tumors by malignant potential and may offer some prognostic information:
- Carcinoma in situ
- Complex carcinoma
- Simple carcinoma (i.e., tubulopapillary, solid, and anaplastic)
- Special carcinoma types (i.e., spindle cell, mucinous, lipid-rich, and SCC)
- Sarcoma (i.e., FSA, OSA, and other)
- Carcinosarcoma
- Carcinoma or sarcoma in benign tumor
- Secretory carcinoma is a rare mammary tumor characterized by the presence of intracellular and extracellular eosinophilic excretions
- Sarcomas are uncommon and may arise from myoepithelial tissue which have undergone malignant change or from intralobular connective tissue
- Sarcomas do not arise from preexisting benign mixed mammary tumors
- Malignant tumors metastasize by hematogenous and lymphatic routes
- Metastatic sites: regional lymph nodes, lungs, adrenal gland, kidney, heart, liver, bone, brain, and skin
- Metastasis to the lungs is more common with primary tumors in mammary glands 4-5
+ Inflammatory Carcinoma
- Inflammatory mammary carcinomas account for 4%-18% of malignant mammary tumors
- Inflammatory mammary carcinomas are poorly differentiated with extensive mononuclear and leukocyte cellular infiltrates, edema, rapid growth and metastasis, and invasion of cutaneous lymphatics with marked edema and inflammation
- Primary and secondary inflammatory mammary carcinomas:
- Primary: acute onset of inflammatory signs
- Secondary: inflammatory signs develop after excision of mammary tumor or present for > 4 months
- Dogs with inflammatory mammary carcinoma were significantly older than dogs with other mammary tumors
- Development of inflammatory carcinoma is associated with diestrous phase of the estrous cycle and hence progesterone may play a direct or indirect role in the development of inflammatory mammary carcinomas
- 96% have regional lymph node and 32% have thoracic metastasis at diagnosis, and 100% have regional lymph node and 62% have thoracic metastasis at euthanasia
- Primary inflammatory mammary carcinomas have a poorer prognosis than other mammary tumors with a more aggressive behaviour, faster growth rate, and poor clinical condition
+ Ovariohysterectomy
- Reduces the risk of mammary neoplasia with an incidence of 0.5% if before neutered before the 1st estrous, 8% before the 2nd estrous, 26% after 2 ovarian cycles, and no protective effect after 2.5 years
- Ovariohysterectomy is not indicated if > 2.5 years as does not affect biologic behaviou
+ Hormones and Hormonal Receptors
- Estrogen and progesterone receptors are present in 70% of benign and 50% of malignant mammary tumors
- Tumors which lack of hormone receptors are more aggressive and less differentiated
- EGF and TGF are associated with estrogen and progesterone receptors and may play a role in the development of mammary tumors
+ Exogenous Progestins
- Progesterone and synthetic progestins (i.e., medroxyprogesterone acetate) induce lobuloalveolar development of mammary glands with hyperplasia of secretory myoepithelial elements
- Exogenous progestins stimulate multiple benign nodules
- Estradiol stimulates ductal growth, but has not been associated with mammary tumor development
- Mammary tumor risk increases with the combined use of estrogens and high dose progestins or drugs with combined progestagenic-estrogenic activity
- Norwegian Canine Cancer Register 1990-1998: 25% of bitches and 5% dogs with mammary tumors were treated with medroxyprogesterone acetate
- 19-nortesterone causes mammary carcinoma in 40% of treated dogs
- Exogenous progestins induce growth hormone production which may influence mammary gland tumor development by proliferation and transformation of susceptible mammary epithelial cells
+ Diet
- High fat diet and obesity increase the risk of mammary tumor development in dogs, rodents, and humans
- Risk of mammary neoplasia is lower if dogs are thin at 9-12 months
- Obesity at 12 months is a risk factor for development of mammary tumors
- Nutritional factors may also play a role as home-made meals (high in beef and pork and low in chicken) are associated with an increased risk of mammary neoplasia
CLINICAL SIGNS
+ General Considerations
- Single or multiple masses within the mammary chain developing simultaneously or subsequently
- Mammary mass can be associated with glandular tissue (common) or nipple
- 65%-70% mammary neoplasia occurs in mammary glands 4 and 5 due to greater volume of mammary tissue
- Benign tumors are often small, well-circumscribed, and firm
- Malignant tumors often have rapid growth, ill-defined borders, fixation to skin or underlying tissue, and ulceration or inflammation
- Inguinal lymph node metastasis can spread via pudendal lymphatics to sublumbar lymph nodes and cause tenesmus
- Vesicopustular dermatitis is associated with cutaneous metastasis from mammary carcinosarcoma
+ Inflammatory Mammary Carcinoma
- Clinical signs: pain, anorexia, weight loss, generalized weakness, and polyuria-polydipsia
- Inflammatory mammary carcinomas were apparent significantly earlier after the last estrus (52 days v 137 days) and is associated with diestrous phase of the estrous cycle and hence progesterone may play a direct or indirect role in the development of inflammatory mammary carcinomas
- Inflammatory carcinomas are diffusely swollen with poor demarcation between normal and abnormal tissue
- Physical examination findings: diffuse involvement of both mammary chains in 55%, palpable mammary mass in 24%, and pelvic limb edema and lameness in 61%
- Lymphedema in the pelvic limb adjacent to inflammatory carcinoma can be observed due to occlusion of lymphatics and retrograde growth of tumor
- DDx: acute mastitis (localized and associated with estrous or false pregnancy compared to firm and diffuse swelling)
DIAGNOSIS
+ General Considerations
- Physical and rectal examination to assess extent of disease
- Hematology and serum biochemistry
- Coagulation profile is recommended in dogs with suspected malignant tumors due to the risk of DIC
- FNA but difficult to differentiate benign and malignant mammary tumors
- FNA is useful in the diagnosis of inflammatory carcinoma and metastatic mammary tumors to regional lymph node
- Thoracic radiographs for metastatic disease
- Caudal abdominal radiographs or ultrasonography for sublumbar lymph node metastasis
- Biopsy if inflammatory mammary carcinoma is suspected
- Ultrasonography: benign tumors have regular margins and are spherical-to-ovoid shaped with a homogenous echogenic pattern while malignant tumors have irregular margins with heterogenous internal echogenicity
MEDICAL MANAGEMENT
+ Chemotherapy
- No known effective adjuvant chemotherapy protocol for malignant or metastatic mammary tumors
- Doxorubicin and cyclophosphamide or cisplatin has some antitumor effect against mammary ADC
- Doxorubicin associated with PR with duration of 12 and 15 months in 2 dogs with metastatic mammary ADC
- Doxorubicin has better efficacy than platinum drugs and carboplatin and cisplatin have equivalent efficacy in vivo and efficacy was not affected by cell type (i.e., ADC, solid carcinoma, and mixed )
- 5-fluoroucil and cyclophosphamide combination significantly improves survival time in dogs with high-risk mammary carcinomas following surgical resection compared to surgery alone (MST 24 months v 6 months)
- Piroxicam combined with radiation therapy is the best treatment for dogs with inflammatory mammary carcinoma
- Bisphosphonates and palliative radiation therapy for metastatic bone lesions
+ Radiation Therapy
- Role of radiation therapy with incompletely resected mammary tumors has not been investigated
- Short-term regression reported for radiation therapy in dogs with inflammatory mammary carcinoma
+ Immunotherapy
- Non-specific immunomodulation with levamisole and Corynebacterium parvum with BCG combined with surgery has no significant effect compared to surgery alone
- Liposome-encapsulated muramyl-tripeptide phosphatidylethanolamine, a derivative of mycobacterial cell wall, is not effective in dogs with invasive mammary carcinoma
+ Hormonal Therapy
- Hormonal therapy is controversial
- Hormonal therapy may be ineffective due to lack of steroid receptors in malignant mammary tumors
- Hormonal therapy may be indicated for tumors expressing estrogen, progesterone, or prolactin receptors
- Tamoxifen is a mixed anti-estrogen with both agonist and antagonistic effects which are species dependent
- Tamoxifen is used in women with estrogen receptor-positive breast cancers
- Tamoxifen has antiproliferative activity in vitro and limited degree in vivo with response in 0% (0/10) and 71% (5/7) dogs with inoperable and metastatic tumors, respectively
- Mean survival time 4 months
- Adverse effects preclude routine use: vulvar swelling, vaginal discharge, incontinence, UTI, stump pyometra, and signs of estrous
- LHRH analogue (Goserilin) reduced circulating levels of estradiol and progesterone and had some antitumor activity in 53% (18/34) dogs with estrogen receptor-positive mammary carcinoma
SURGICAL MANAGEMENT
+ General Considerations
- Surgical excision of mammary tumors is recommended
- Contraindications: metastatic disease or inflammatory carcinoma
- Inflammatory carcinoma often advanced at diagnosis and recurrence common
- Excisional techniques include: excisional biopsy, local mastectomy, regional mastectomy, unilateral mastectomy, and simultaneous or staged bilateral mastectomy
- No difference in recurrence rate or survival time of simple mastectomy and radical mastectomy
- Radical surgery may reduce risk of de novo tumor development and malignant transformation of benign lesions, however, radical mastectomy is associated with greater morbidity and over-treatment for both benign and malignant mammary tumors
- Aim: removal of all neoplastic tissue with simplest procedure
- ± ovariohysterectomy
+ Excisional Biopsy
- Indications: small (< 0.5 cm), firm, superficial, and non-fixed mammary masses
- Excisional biopsy is preferred with removal of a margin of normal tissue and 2-layer closure
- Wide excision is recommended with feline mammary tumors due to malignancy
+ Local Mastectomy
- Indications: centrally located lesions, lesions > 1.0 cm, and masses with any degree of fixation
- Local mastectomy is the removal of a single mammary gland
- 2 elliptical incisions performed around the mammary gland
- Soft tissue dissection to the abdominal wall with muscular fascia included in the resected tissue
- Enlarged lymph node is removed or normal lymph node is biopsied for metastatic disease
- 2 layer closure
+ Regional Mastectomy
- Regional mastectomy is the removal of ≥ 2 mammary glands and associated lymph nodes
- Regional mastectomy was originally proposed based on the venous and lymphatic drainage of mammary glands
- Mammary glands 1, 2, 3 ± 4 drain into axillary and cranial sternal lymph node
- Mammary glands 3, 4, 5 ± 2 drain into superficial inguinal lymph node
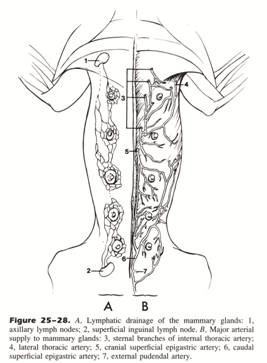 From: Slatter DH (ed): Textbook of Small Animal Surgery (3rd ed).
From: Slatter DH (ed): Textbook of Small Animal Surgery (3rd ed).
- superficial inguinal lymph node has efferent drainage to medial iliac lymph node, lumbar trunk, and cisterna chyli
- indications: large mammary masses in adjacent glands
- dissection similar to local mastectomy
+ Unilateral Mastectomy
- Unilateral mastectomy is the removal of 1 entire mammary chain
- Indications: multiple mammary masses involving ≥ 2 ipsilateral mammary glands
- 2 elliptical incisions performed ending cranial to gland 1 and caudal to gland 5 near the vulva
- Soft tissue dissection to the abdominal wall with muscular fascia included in the resected tissue
- Sissection begun at gland 5 as ligation of caudal superficial epigastric reduces hemorrhage
- Allis tissue forceps placed on gland 5 and sharp and blunt dissection used to elevate mammary chain
- Caudal superficial epigastric artery and vein are ligated and divided
- Plane of dissection is less defined at the paracostal arch
- Superficial inguinal lymph node is located in the inguinal fat pad
- Axillary lymph node is located immediately ventral to the latissimus dorsi muscle near the lateral thoracic artery
- 2 layer closure ± penrose drain
- Postoperative management: analgesia for 24 hours and non-adherent bandage and stockingette
+ Staged Bilateral Mastectomy
- Staged procedure: unilateral mastectomy 6 weeks apart
- Advantages: closure easier due to skin stretch and each procedure shorter than bilateral alone
- Staged procedures preferred in breeds with less skin for closure (i.e., Greyhound and Dachshund)
- disadvantage: 2 general anesthetics and surgeries are required
+ Simultaneous Bilateral Mastectomy
- Indications: multiple and bilateral mammary gland involvement in otherwise healthy dogs
- Assess skin pliability before attempting simultaneous procedure by grasping lateral margins and moving them medially towards then ventral midline while in dorsal recumbency
- Dissection similar to unilateral mastectomy except triangular skin over xyphoid is preserved
- Wound closure: walking sutures, intradermal sutures from caudal to cranial, and simple interrupted sutures
- Stent sutures may be required near the xyphoid process where tension is the greatest
- Wound dehiscence is common and tension relieving techniques should be considered
- Postoperative management the same as unilateral mastectomy
PROGNOSIS
+ General Considerations
- poor prognostic factors include:
- tumor size > 3cm
- ulceration
- histologic grade and type
- degree of nuclear differentiation
- lymphoid cellular reactivity in tumor vicinity
- degree of invasion
- intravascular growth
- steroid hormone receptor activity (i.e., no estrogen receptors)
- DNA aneuploidy
- S-phase fraction as measure of cellular proliferation
- AgNOR counts
- metastatic disease to regional lymph nodes and distant sites
+ Tumor Size
- MST is significantly better for tumors < 5 cm (i.e., stage I and II disease) (MST 112 weeks v 40 weeks)
- MST is significantly better for tumors < 3 cm (i.e., stage I disease) (MST 22 months v 14 months)
- Local tumor recurrence rates are significantly better for dogs with tumors < 3 cm at 1-year (30% v 70%) and 2-years (40% v 80%)
+ Clinical Stage
- MST for dogs with stage I disease is significantly better than stage II-IV disease (24 months v 12 months for stage II, 15 months for stage III, and 19 months for stage IV disease)
- MST is dependent on clinical stage:
- MST 500 days for stage I mammary tumors
- MST 420 days for stage II mammary tumors
- MST 210 days for stage III mammary tumors
- MST 90 days for stage IV mammary tumors
+ Histologic Type
- Carcinomas have a better prognosis than sarcomas
- Majority of dogs with mammary sarcomas die from tumor-related causes within 9-12 months
- Carcinoma subtypes have prognostic importance with ductular carcinoma and carcinosarcoma associated with a poorer prognosis
- True carcinomas have a higher metastatic rate (100%) than ADC in mixed mammary tumors (34%)
- Ductular carcinomas have a higher rate of metastasis and mortality
- Mortality rates: 20% lobular ADC, 65% ductular ADC and 15% for other mammary ADC
- MST for anaplastic carcinoma (2.5 months) is significantly decreased compared to ADC (21 months), solid carcinoma (16 months), and other mammary tumors (14 months)
- Carcinosarcoma and inflammatory mammary carcinoma associated with 100% fatality
- MST 25 days for inflammatory mammary carcinoma
- Infiltration of carcinoma into adjacent tissue is associated with a poor prognosis
+ Histologic Grade
- Carcinoma in situ
- Invasion of surrounding stroma without vascular or lymphatic invasion
- Vascular or lymphatic invasion or regional lymph node metastasis
- Distant metastasis
- Histologic grade and degree of differentiation are significantly related to tumor aggressiveness
- 19% of grade 0, 60% of grade 1, and 97% of grade 2 mammary tumors have recurrence or metastasis within 2 years of mastectomy
+ Nuclear Differentiation
- Mammary tumors are further classified based on degree of nuclear differentiation: poor, moderate, and well
- Local tumor recurrence in 24% of grade 1, 68% of grade 2, and 90% of grade 3 mammary carcinomas
+ Lymphoid Cellular Reaction
- Lymphoid cellular reaction in tumor vicinity may represent immunologic antitumor response
- Local tumor recurrence and metastasis is more common in dogs without lymphoid cellular reaction in tumor vicinity
- 45% of grade 1 mammary tumors with lymphoid cellular reactivity have recurrence within 2 years v 83% of grade 1 mammary tumors without lymphoid cellular reactivity
+ Estrogen Receptors
- Presence of estrogen receptors above a certain threshold associated with improved postoperative survival
- However, estrogen receptors are associated with degree of differentiation
- Estrogen expression significantly decreased with increased tumor size, ulceration, lymph node metastasis, and malignant histology, and is inversely correlated with PCNA index
+ Hemostatic Abnormalities
- ≥ 1 hemostatic abnormality in 67% dogs with mammary carcinoma and incidence increases with histologic grade
- Hemostatic abnormalities are more common with metastasis, extensive necrosis, inflammatory carcinoma, fixed tumors, or histologic evidence of penetration of tumor capsule
- Abnormal hemostatic parameters include platelet count, PT, APTT, thrombin time, plasma activity of factors V, VIII and X, plasma concentrations of fibrinogen, fibrin monomers and FDP, and AT-III
+ Ovariohysterectomy
- Effect of ovariohysterectomy on local tumor recurrence and survival is controversial
- Ovariohysterectomy concurrently with mastectomy or within 2 years of mastectomy for dogs with mammary carcinoma significantly increases survival time, with a MST of 755 days v MST 286 days for dogs spayed > 2 years before mastectomy and MST 301 days for intact dogs without concurrent ovariohysterectomy, and increased survival time by 45%
- MST between dogs with mastectomy and dogs with mastectomy and ovariohysterectomy are not statistically different (8 and 10 months compared to 8.4 months)
- However, other studies show ovariohysterectomy does not improve tumor-related or overall survival time in dogs with mammary tumors treated with mastectomy (8.4 months v 8-10 months)
+ Lymph Node Metastasis
- Controversial as not a significant factor in multivariate analysis but is a significant factor in univariate analysis
- Lymph node involvement is associated with significantly DFI (6-month local tumor recurrence rate 80% v 30%) and survival time
- MST is significantly decreased with metastatic disease (5 months v 28 months)
+ Other
- High fraction of cells in the S-phase and DNA aneuploidy is associated with reduced survival times in 136 dogs
- Ki67 labeling index is associated with poor prognosis
- AgNOR counts are associated with cellular proliferation and hence high counts associated with poor prognosis
- Proliferative cell nuclear antigen (PCNA) index is highest in malignant tumors (16%-27%) compared to benign tumors (4.4%-5.3%), mammary hyperplasia (2%), and normal mammary tissue (1%)
- c-erbB-2 over-expression is associated with development of metastatic disease and may be important for development of malignancy
- Telomerase activity is significantly higher in dogs with mammary ADC than benign mammary tumors, but telomerase activity is not present in malignant mammary mixed tumor
- Malignant mammary tumors without progesterone receptors proliferate at a higher rate than malignant tumors with progesterone receptors
MAMMARY
TUMORS
| T0 | No evidence of neoplasia | T1 | Tumor < 3 cm in diameter - Primary Tumo | T2 | Tumor 3-5 cm in diameter |
| T3 | Tumor > 5 cm in diameter | N0 | No evidence of lymph node involvement |
| N1 | Regional lymph node involvement - Node |
| M0 | No evidence of metastasis |
| M1 | M1 Evidence of distant metastasis with site specified - Metastasis |
clinical stage
| I | II | III | T | T1 | T2 | T3 | N | N0 | N0 | N0 | M | M0 | M0 | M0 | IV | T1-3 | N1 | M0 | V | T1-3 | N0-1 | M1 |


