GENERAL CONSIDERATIONS
+ Cats
- Epithelial neoplasms are the most common metastatic tumor in cats
- Survey radiographs: ill-defined pulmonary nodules, alveolar disease, pleural effusion, and a combination of these are the most common findings in cats with metastatic disease
- Mammary carcinomas often have ill-defined nodules or a diffuse pulmonary pattern
- Alveolar pattern observed in metastatic mammary and pulmonary neoplasia is due to confluence of smaller tumor nodules, hemorrhagic or necrotic reaction of lung parenchyma to tumor emboli, pulmonary edema secondary to airway obstruction by tumor, or extension of tumor into alveolar spaces
+ Dogs
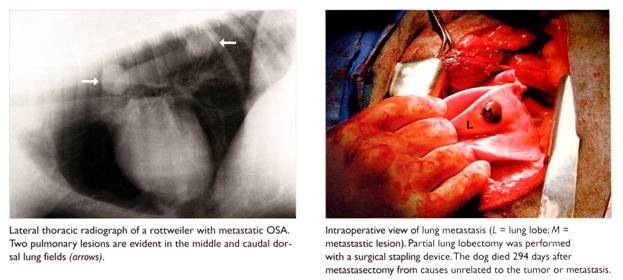
- Pulmonary metastatic disease most commonly presents as multiple circumscribed interstitial nodules
- Diffuse reticulonodular or alveolar pattern is occasionally described for pulmonary LSA, metastatic mammary carcinoma, and diffuse alveolar carcinoma
- Ill-defined coalescing nodules or alveolar infiltrates in dogs with metastatic HSA secondary to hemorrhage
CONSERVATIVE MANAGEMENT
+ Chemotherapy
- Chemotherapy has no benefit as MST following single-agent cisplatin chemotherapy is 61 days for dogs with metastatic OSA
- Inhalant chemotherapy using paclitaxel or doxorubicin has been investigated in dogs with primary and metastatic lung tumors:
- Responses in sarcomas but not carcinomas to doxorubicin
- Responses in both sarcomas and carcinomas with paclitaxel
- Response rate 27% (6/22) with 22.5% PR (5/22) and 4.5% CR (1/22)
- Intermittent and non-productive cough for 1-10 days in 50% dogs following inhalant doxorubicin
- Allergic reactions common following paclitaxel administration
+ Gene Therapy
- Advantages: target production of therapeutic protein to lung or lung tumor, avoid systemic toxicity and achieve sustained protein production with less frequent treatments
- Vector systems for lung tumors: adenovirus vectors and plasmid-DNA-lipid complexes (or lipocomplexes)
- Routes for gene therapy: direct tumor injection into tumor, intratracheal administration for pulmonary epithelium, and intravenous delivery for pulmonary epithelium
- Direct intratumoral injection of bacterial superantigen with cytokine gene (GM-CSF or IL-2) induces PR or CR in 46% (12/46) of dogs with metastatic pulmonary OSA
SURGICAL MANAGEMENT
+ Pulmonary Metastatectomy
- Indications for pulmonary metastatectomy include:
- Metastasis-free interval > 300 days
- Prior exposure to effective chemotherapy
- No other known metastatic sites,
40 day doubling time of metastatic lesions
- < 3 radiographically visible metastatic lesions
- Palliative treatment of dogs hypertrophic osteopathy
- Majority of metastatic lesions are located either in the peripheral or subpleural portions of the lung and preservation parenchymal tissue preferred to prevent respiratory and cardiovascular compromise
- 33% of dogs have more metastatic lesions detected intraoperatively than indicated by thoracic radiographs
- Prognosis: MST 176 days and 1-year survival rate 28%
- Median DFI significantly better for dogs with > 300 day metastasis-free interval (128 days v 58 days)
- Median DFI significantly better for dogs with 1-2 metastatic nodules (95 days v 53 days)
From: Liptak JM, et al: Canine appendicular osteosarcoma: curative-intent treatment. Compend Contin Educ Pract Vet, 26:186-197, 2004.


