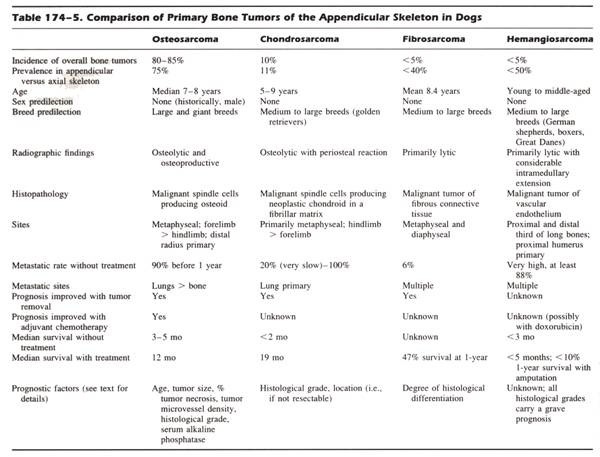
GENERAL CONSIDERATIONS
+ Malignant Primary Bone Tumors
- Bone tumors can arise from tissue elements within the bone (i.e., primary) or secondarily invade bone by either local extension or distant metastasis (i.e., secondary)
- Primary bone tumors are more common and often malignant
- Primary malignant bone tumors include OSA, CSA, FSA, and HSA ± undifferentiated sarcoma and liposarcoma
- OSA is the most common primary bone tumor in dogs and accounts for 85%-98% of bone tumors and 2%-7% of all canine tumors
 From: Slatter DH (ed): Textbook of Small Animal Surgery (3rd ed).
From: Slatter DH (ed): Textbook of Small Animal Surgery (3rd ed).
Bone tumors have a different presentation and distribution in dogs < 15 kg:
- Mean age 10.5 years is significantly older than large breed
- OSA accounts for 43% of bone tumors
- Ratio of axial-to-appendicular sites is 1:1 in small breed dogs v 1:5 in large breed dogs
- Femur is the most common appendicular site v distal radius in large breed dogs
- OSA is 20-times less likely to occur in small breed dogs
- FSA is 2nd most common primary bone tumor in small breed dogs
- 70% of primary bone tumors occurred in the axial skeleton v 28% in large dogs
- 24% of bone tumors are metastatic tumors, especially from bladder TCC and mammary ADC, v 5% in large breed dogs
+ Benign Primary Bone Tumors
- Primary benign bone tumors include osteoma, endochrondroma, multiple cartilaginous exostoses, and chondroma
- Osteoma is a slowly progressive growth with no metastasis or malignant transformation
- Endochrondroma is a medullary cartilaginous tumor with no metastasis or malignant transformation in animals
- Multiple cartilaginous exostoses is characterized by mono- or polyostotic cartilage tipped protuberances from bone which stop growing with skeletal maturity in dogs, but not cats
- Multiple cartilaginous exostoses may be hereditary and malignant transformation is relatively common
+ Other Bone Tumors
- Tumors that secondarily involve bone include multiple myeloma and LSA
- Tumors that invade bone include:
- STS
- Oral SCC, malignant melanoma, and FSA
- Digit SCC and malignant melanoma
- Tumors with a propensity to metastasize to bone include:
- Pulmonary carcinoma in cats
- Urothelial (i.e., bladder TCC and prostate carcinoma) and mammary carcinomas in dogs
CLINICAL SIGNS
Appendicular Skeleton
+ General Considerations
- Pain and lameness are the most common signs of appendicular bone tumors
- Pain is caused by microfractures or disruption of the periosteum with extension of the tumor
- Palpable swelling or mass may not be evident
- Swelling is usually caused by extracompartmental extension of the bone tumor into adjacent soft tissue
- Response to deep palpation is essential to differentiate from osteoarthritis and cranial cruciate ligament rupture
- Lameness is gradual in onset and progressive (due to subperiosteal hemorrhage and cortical microfractures) with no worsening after exercise
- OSA should be considered with any lameness of the metaphyseal area in large to giant breeds
+ Pathologic Fracture
- Acute onset of non-weight bearing lameness with pathologic fracture but accounts for < 3% of all fractures
- Osteolytic tumor cells cause pain, hypercalcemia, bone marrow replacement, alter biomechanical properties, and can cause pathologic fractures
- Osteolysis begins in the medullary canal and extends to the endosteal surface of the cortex resulting in compromised structural integrity and the risk of pathologic fracture due to deterioration in bone mass, architecture and strength
- Tumor implanted bone has an 11% decrease in bone mineral content, 9%-11% decrease in bone mineral density, 35%-41% decrease in failure torque, and 35%-39% decrease in torsional stiffness
+ Metastases
- Inappetence and malaise are the most common symptoms
- Hypertrophic osteopathy may develop in dogs with pulmonary metastases
- Respiratory signs uncommon
+ Radiation-Induced Sarcoma
- Radiation-induced OSA usually associated with high dose-fraction schemes (> 3.5-5.0 Gy/fraction)
- Criteria for radiation-induced OSA:
- No radiographically detectable lesion prior to radiation therapy
- OSA in the radiation-field
- Tumor type confirmed histologically
- Long asymptomatic period radiation therapy and tumor detection
- Tumor normally occurs with a low incidence at the site
DIAGNOSIS
Regional Radiographs
+ Primary Bone Tumors
- Survey radiographs are necessary to differentiate tumors from fractures, osteomyelitis, and metabolic bone diseases
- 3 basic types of OSA: endosteal (very common), periosteal, and parosteal
- Radiographic findings consistent with endosteal bone tumors include mixture of lytic changes (due to cortical destruction and loss of trabecular detail) and blastic changes (due to periosteal proliferation, new bone production, and sclerosis)
- Soft tissue extension with new tumor bone development produces a palisading pattern perpendicular to or radiating from the axis of the cortex (= sunburst effect)
- Tumor invasion of the cortex elevates the periosteum with new bone formation from the cambium layer resulting in a triangular deposition of dense new bone at the periphery and on the cortex (= Codman's triangle)
- Other radiographic findings include:
- Loss of fine trabecular pattern in the metaphysis
- Vague transition zone at the extent of the lesion (v sharp sclerotic margins) with poorly defined margin
- Fine punctate lysis
- Pathologic fracture with metaphyseal collapse
- Periosteal and parosteal OSA originate from the periosteal surface of the bone and rarely involve the endosteum and medullary canal
- Parosteal OSA has an irregular shape with smooth border and arises from the bone surface without affecting the cortical bone and, especially in humans, there may be a thin translucent line between tumor and normal underlying bone (better appreciated with CT)
- Appendicular FSA and CSA have a similar radiographic appearance to OSA and cannot be differentiated radiographically, whereas HSA often has a lytic radiographic appearance
+ Osteomyelitis
- Mycotic osteomyelitis is the major differential diagnosis for primary bone tumors as fungal lesions can be monostotic with a preference for the metaphyseal region of long bones
- Coccidioides immitis and Blastomyces dermatitidis are the most common fungal agents with bone involvement
- Coccidiomycosis is endemic in SW USA and blastomycosis is endemic in SE USA
- History is necessary to determine whether the dog lives or has traveled through an area endemic for fungal disease
- Majority of mycotic osteomyelitis can be differentiated from primary bone tumors by polyostotic bone involvement (more common than monostotic) and symptomatic illness associated with pulmonary infiltrates and thoracic lymphadenomegaly
- DDx: bacterial osteomyelitis, atypical bone cysts, and metastatic neoplasia
+ Thoracic Radiographs
- Appendicular OSA is a highly malignant tumor with < 15% dogs having clinically detectable metastasis at the time of initial diagnosis, but 75%-90% eventually developing metastatic disease
- Metastasis occurs primarily through hematogenous routes, particularly to the lungs and other bone, but a 25% rate of metastasis to regional lymph nodes is also reported
- Palpation of regional lymph nodes, thoracic radiographs, and nuclear scintigraphy are for staging of dogs ± cats with suspected primary bone tumors
- 3-view thoracic radiographs, including right and left lateral and ventrodorsal projections, are required for the diagnosis of pulmonary metastases
- Right and left lateral projections are important as the non-dependent lung fields are better aerated and closer to the anode, resulting in better contrast and magnification, respectively, of metastatic lesions
- Metastatic lesions ≥ 6 mm diameter can be detected with good-quality radiographs
- Smaller lesions can be visualized with greater sensitivity using CT scans (additional 10%-20%), but advanced imaging is expensive and associated with a high rate of false-positive diagnoses
+ Nuclear Scintigraphy
- Indication: metastasis evaluation and surgical planning for limb-sparing surgery
- whole-body bone scans, using radiolabeled technetium pertechnetate, are sensitive for the detection of skeletal abnormalities, including both primary and metastatic tumors, but not specific
- bone scintigraphy cannot differentiate benign from malignant or detect pulmonary metastases
- 2nd asymptomatic bone lesion, consistent with metastatic disease, is identified in 4%-28% of dogs with OSA
- survey radiographs of 2nd lesions should be performed to confirm the presence of bone pathology
- Survey radiographs of the skeleton, consisting of lateral radiographs of long bones and ventrodorsal radiographs of the pelvis, is an alternative to screen for bone metastases if nuclear scintigraphy is unavailable
Bone Biopsy
+ General Indications
- Histopathology required for definitive diagnosis of bone tumor
- Biopsy techniques include FNA, closed (i.e., Jamshidi needle), limited open (i.e., Michele trephine), or open
- Biopsy sites should be planned from regional radiographs
- Bone biopsy = core biopsy (i.e., near cortex and medullary cavity) of the central and transitional zones of the tumor
- Definitive diagnosis of bone tumor is obtained in 83.9% of central biopsy and 54.5% of transitional biopsy samples
- Biopsy should be performed by same person performing definitive surgery so that:
- Biopsy tract can be excised en bloc with the tumor at definitive surgery
- No additional compartments or neurovascular structures are contaminated as a result of either manipulation or hematoma formation
- Ideal sample should be 1-2 cm in length and not fragmented
- Bone biopsy samples should be submitted for cytology and culture and sensitivity
- Biopsy result of reactive bone or bone tumor other than OSA should be considered with caution as > 50% are OSA
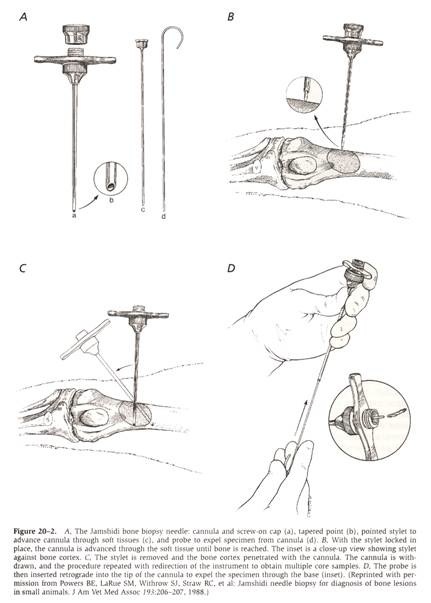 From: Withrow SJ & MacEwen EG (eds): Small Animal Clinical Oncology (3rd ed).
From: Withrow SJ & MacEwen EG (eds): Small Animal Clinical Oncology (3rd ed).
+ Ultrasound-Guided Fine-Needle Aspiration
- Ultrasonographic examination of bone possible if cortical defects are present
- Aspiration of the intramedullary region can be performed through areas of cortical destruction
- Advantages: improved sampling technique, biopsy without general anesthesia or sedation, quicker results and tissue-core biopsy can be performed if FNA unsuccessful
- Disadvantage: multiple aspirates are often required for a definitive diagnosis, excessive blood contamination can interfere with cytologic evaluation (particularly with low cellularity), and cortical bone destruction must be present
- Small gauge hypodermic needle (22 G) is preferred as larger gauge results in significant hemodilution
- 93% sensitivity for ultrasound-guided FNA of bone lesions in humans
- Bone tumor is correctly diagnosed in 11/23 (48%) dogs with 5 unsuccessful due to poorly exfoliating sarcomas
+ Jamshidi Needle Biopsy
- Multiple central biopsies (i.e., 2-4 core biopsies) can be obtained with a Jamshidi needle core biopsy
- Biopsy should only include the cis-cortex and medullary cavity and not the trans-cortex
- Jamshidi core biopsies have a diagnostic accuracy of 82.3% for tumor type and 91.9% for differentiating tumor from other causes
- Potential problems include incorrect diagnosis due to heterogenous tumor or sampling of surrounding bone, iatrogenic fracture, and incorrect placement if limb-spare surgery is planned
+ Michele Trephine
- Open technique ensures large sample size but increases risk of operative complications (i.e., hematoma, infection, dehiscence, tumor seeding, and pathologic fracture)
- Limited open technique with a Michele trephine results in a diagnostic accuracy of 93.8% but increases the risk of pathologic fracture compared to Jamshidi needle (3%)
- Diagnostic accuracy depends on histopathologic type of tumor with an 81%-84% accuracy for OSA and 29%-39% accuracy for non-OSA
+ Clinical Staging
- Clinical staging is confined to bone and presence of metastatic disease as regional lymph node involvement is rare
- Human staging system: histologic grade (G), primary tumor site (T) and regional or distant metastases (M)
- Stage I: low grade (G1) without metastases
- Stage II: high grade (G2) without metastases
- Stage III: regional or distant metastases regardless of grade
- T subdivided into A (intracompartmental) and B (extracompartmental)
TREATMENT PLANNING
From: Slatter DH (ed): Textbook of Small Animal Surgery (3rd ed).



